Swayback Posture & Therapy by Dr. Jeffrey Tucker
Dr. Jeffrey Tucker
11620 Wilshire Blvd. #710
Los Angeles, CA 90025
310-444-9393
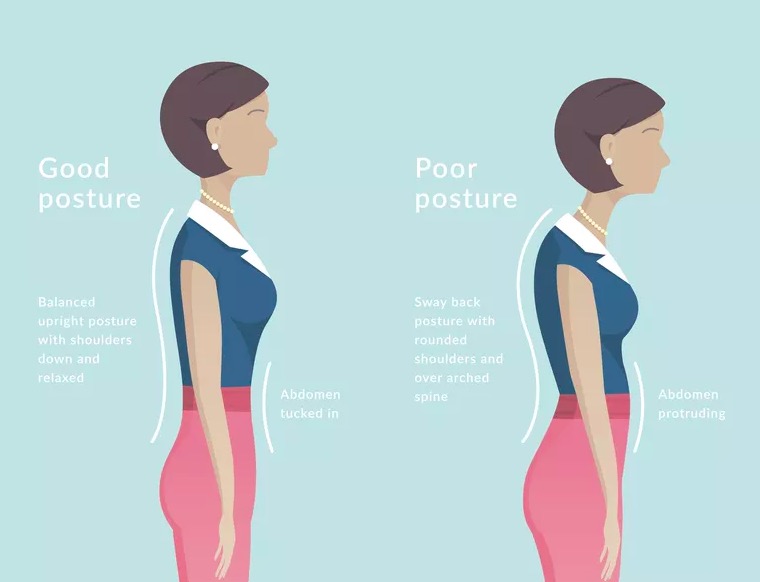
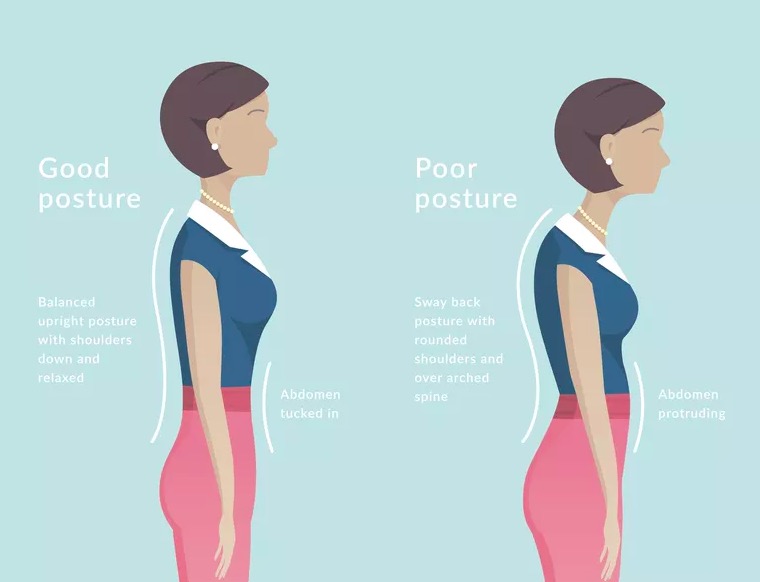
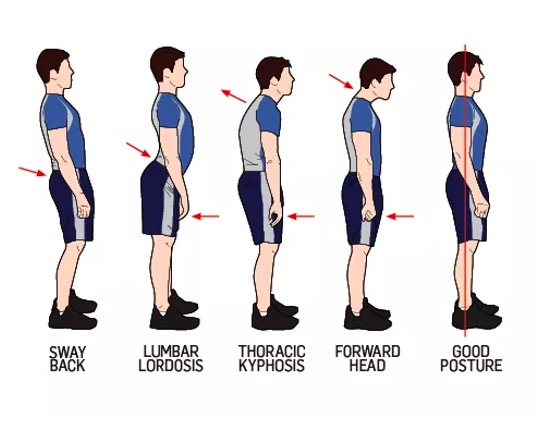
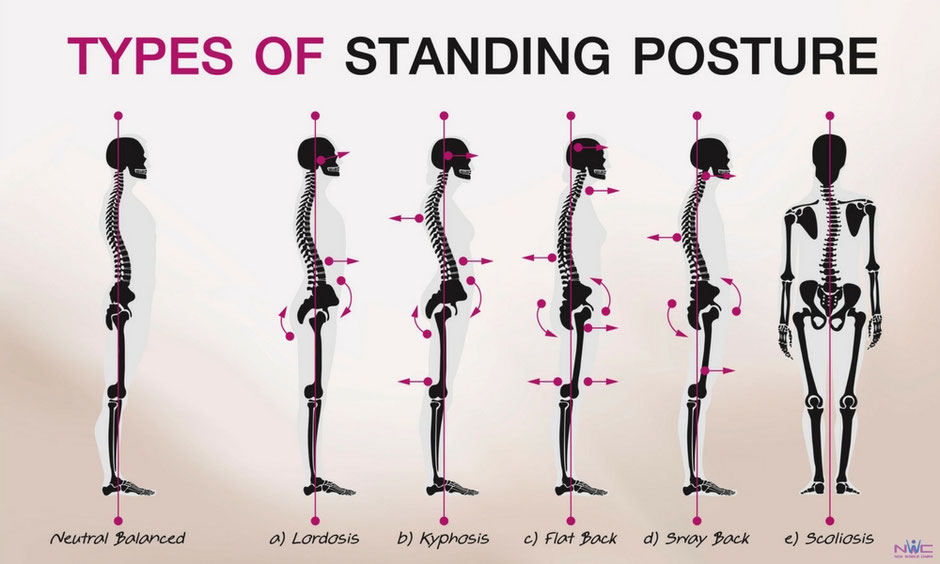
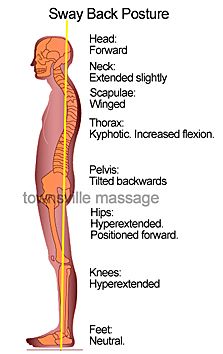
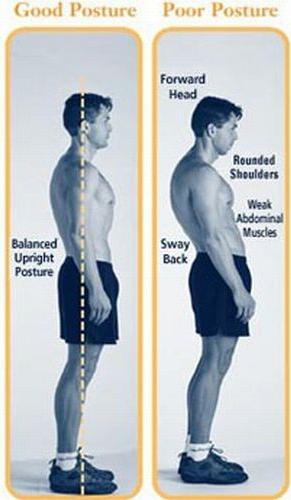
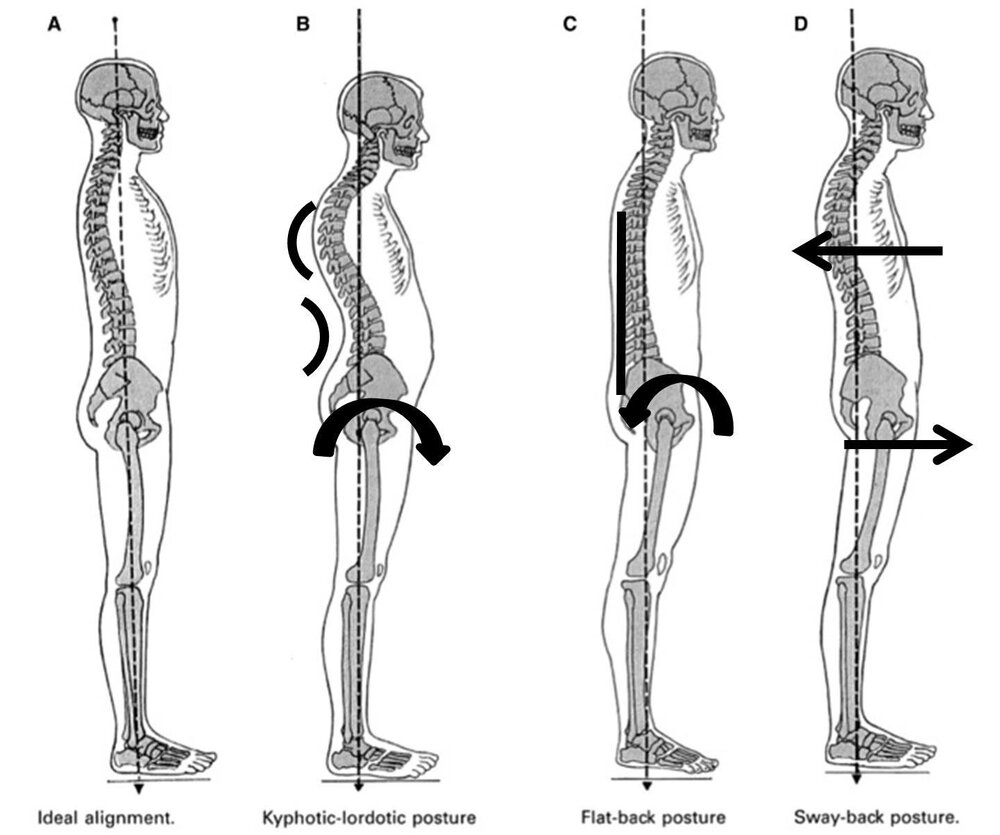
Swayback refers to the low lumbar area as flattened; the concave curve of the lower spine is much higher, in the lower thoracic spine; the pelvis is tilted posteriorly; the plumb line of the greater trochanter is anterior to the lateral malleolus, revealing the hips and pelvis are swayed forward in the sagittal plane (Kendall 2005); the rib cage is swayed backward in the sagittal plane (Sahrmann 2002).
Swayback posture is common in individuals that are sedentary and sit for prolonged periods of time, older adults with weak gluteal muscles, runners, and ballerinas (Sahrmann 2002). Those with swayback frequently present to chiropractors with chronic low back pain.
Lordotic posture refers to the excessive concave lumbar spine; the pelvis is tilted anteriorly; in both lordotic and ideal postures the greater trochanter is over the lateral malleolus. Hip flexor tightness (Iliopsoas, Quadriceps, Vastus) is common with lordotic posture (Kendall 2005). Visually, the pelvic bowl dips anteriorly, raising the body’s center of gravity. Lordotic postures (Lee, CM, et al. 2001. Biomechanical effects of wearing high-heeled shoes. Int J Ind Ergon, 28(6), 321-326) and sway back can lead to reduced proprioceptive stability. Wearing high heels should be avoided in excessive lumbar lordosis.
How to identify swayback posture from the ground up:
Neutral ankle joint
Hyperextended knees and hips (The femurs create a joint with hyperextended knees and hips)
Posterior pelvic tilt
Anterior deviation of the pelvis over the lateral malleoli
Lower lumbar spine is flattened
Gluteals may look flattened
Caved chest
A long kyphosis (backward curve of the thoracic spine, also known as “hunchback” or rounded upper back) in the posteriorly displaced upper trunk
Forward head posture
Muscle length evaluation reveals short hamstrings (patients perception is ‘tight’ hamstring) and internal oblique muscles with lengthened psoas and external oblique muscles (Kendall 2005).
Muscle strength evaluation reveals dominance of the rectus abdominis over the external obliques (Sahrmann 2002). The gluteals may be atrophied and test weak.
Palpation of the lower rectus abdominis close to the pubic bone attachments often reveals tenderness, tightness, and/or trigger points. This shortening contributes to the posterior pelvic tilt, and the caving of the chest. We should be able to diagnose sway back vs. increased lumbar lordosis by the forward pelvis and the upper torso backward shift (Kendall 2005).
Gait analysis reveals hamstrings dominance over the gluteals to extend the hip. The posterior pelvis tilt puts the gluteals in an abnormal length, causing them to be inhibited, and allowing the hamstrings to take over as the prime movers for hip extension. This alters the length (origin and insertion) of the hamstrings, and the extension they create at the hip puts a torque on the femur, causing the head of the femur to move forward in the hip socket (Sahrmann 2002). Over time and repetition of walking or running loads this can produce significant wear and tear on the anterior area (ligaments, bursa, etc.) of the hip joint and may cause groin pain or hip symptoms. There will also be excess strain on the hamstring tendons especially at the ischial attachments.
Common overuse injuries related to faulty swayback posture include labral tears at the hip, low-back pain, plantar fasciitis, iliopsoas bursitis and tendinopathy, recurrent hamstring strain and shoulder impingement (Sahrmann 2002).
Management:
Manual therapy: Clinically, our hands will never go out of style, and we need to restore physiological vertebral movement and perform manipulation of the apophyseal joints. These patients are stiff especially in the thoracic spine!
Deep Muscle Massager: I have observed that the newly developed Deep Muscle Massager (DMM) made by Dr. Fuji is an excellent complement and ‘patient pleaser’ compared to all other hand held vibration/percussion devices I’ve tried, especially for fascial dysfunction. Dr. Fuji was able to manufacture a cordless, rechargeable and ergonomically designed hand held instrument. The DMM device comes with 3 separate heads for the applicator and offers options of 1 – 5 energy intensity settings. There are two probable primary effects of the Deep Muscle Massager:
1) Direct reaction to the mechanical stimulation.
Indirect stimulation triggering cellular and biochemical processes based on triggering a reactive system.
Direct effects may include the following:
Normalization of the muscle tone through stimulation of the muscle spindle and the Golgi apparatus of the muscle tendon.
Pain overlay based on the gate-control principle (Melzack and Wall) with parallel endorphin release by the stimulation of the skin’s pressure and touch receptors.
Stimulation of cellular activity and changes in cell-membrane permeability caused by direct mechanical stress in the cell wall.
Increased cellular metabolism due to changes in the membrane permeability, e.g. by opening the glutamate channels.
Release of substance P, a neurotransmitter and pain mediator, into the tissue with subsequent nerve habituation and with that reduction of the pain threshold.
Increased cellular activity.
Mechanotransduction i.e. the process of converting physical forces into biochemical signals subsequently integrated into a cellular response (Iqbal and Zaida 2005, Vogel 2006).
I specifically use the Deep Muscle Massager (DMM) for postural distortions to increase venous and arterial flow to the tight muscles and reawakening of underactive muscles. The DMM vibration is also likely to increase metabolite transport into the disc to compliment ↑ imbibition, ↑ Glycosaminolycans, ↑ K, Ca, Mg, Fe, and Na nutrient flow in channels between the vertebral end plates and the disc. The new DMM device is more than an assist in breaking up adhesions and scar tissue; it likely offers mechanoreceptor activation around facet joints (type II); and helps pain mediation by blocking the pain-spasm-pain cycle.
Postural Retraining: This is patient ‘awareness’ of the dysfunction while helping the patient find a more neutral or ‘less threatening’, ‘more stable’, ‘more breath’, ‘more movement’ or whatever you want to call it ‘position’. Be sure they lengthen the torso out through the top of the head and elongate the spine. For patients in pain this will calm the muscles and remove the effects of the spine’s poor position (McGill 2007). My goal is to actually reduce the kyphosis.
Specific Exercises: I use ELDOA exercises to increase IVD space height and facilitate imbibition. The ELDOA exercises complement the DMM and the postural changes I am trying to make to increase the length and size of the discs and spinal canals. Other specific exercises include: side planks and hand/forearm to toes planks. These will shorten and strengthen the external obliques while maintaining length in the internal obliques and rectus abdominis. Bridging and standing single-leg march in place performed slow with arm drivers strengthen the gluteals and psoas while increasing hip mobility and elongating the spine.
Exercise goals:
Increase mobility at the hips, specifically hip flexion.
Increase strength of the gluteus maximus.
Decrease length of the external obliques, and decrease dominance of the rectus abdominis.
Strengthen the short hip flexors (psoas).
I have patients avoid traditional curl-ups, as they continue to build dominance of the rectus abdominis.
Treatment Summary
When working with swayback patients, it is important to emphasize postural cues, Deep Muscle Massager for fascial therapy, and corrective exercise. I constantly remind the patient to stand in a better alignment – active arch (short feet), relaxed knees, pelvis neutral, chest open and in an elongated ‘tall’ position, palms at sides with thumbs facing forward, and no forward head posture.
Dr. Jeffrey Tucker
11620 Wilshire Blvd. #710
Los Angeles, CA 90025
310-444-9393